Hospitals and health systems generate more information today than ever before, yet clarity remains elusive at the moments that matter most. Patient records, billing systems, laboratory platforms, imaging repositories, and connected devices all produce valuable signals, but these signals live in separate environments governed by different rules. Leaders receive reports that explain parts of the story while obscuring others. Teams spend time reconciling numbers instead of acting on them. Decisions slow down, confidence in data weakens, and opportunities for improvement pass unnoticed across clinical, operational, and financial decision-making processes every day.
Healthcare has reached a structural inflection point. Interoperability mandates, value-based reimbursement, and expanding use of artificial intelligence have exposed the limits of fragmented data environments. Architecture has shifted from a technical consideration to a leadership concern. A modern healthcare data architecture now determines how effectively organizations improve outcomes, manage cost, and meet regulatory expectations. Understanding what this architecture looks like in 2025 provides a practical foundation for long-term progress.
Why Healthcare Requires Modern Data Architecture
Legacy healthcare data environments were built to store information, not to support intelligence at scale. Each department optimized its own systems, creating isolated repositories that reflected local priorities rather than enterprise needs. Over time, these silos hardened. Executives received conflicting metrics. Analysts spent more effort cleaning data than analyzing it. Strategic questions took weeks to answer, if they could be answered at all.
A unified architecture replaces fragmentation with reliability. When data enters the organization through standardized pipelines and shared governance, reporting becomes faster and more trustworthy. Regulations such as HIPAA, FHIR, and TEFCA have reinforced the need for traceability, integration, and accountability. The same architectural discipline that supports compliance also improves operational efficiency and patient safety. A sound data foundation now underpins both regulatory readiness and strategic execution.
The Core Layers of Modern Healthcare Data Architecture
A 2025-ready healthcare data architecture functions as a connected system of layers, each with a defined purpose. Together, these layers transform raw data into insight that teams can rely on.
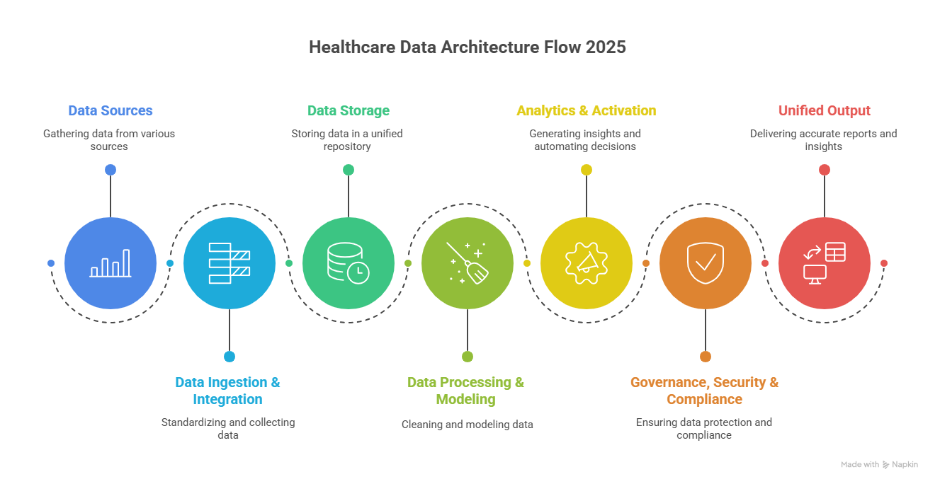
Data ingestion and integration form the entry point. Healthcare organizations manage data from electronic health records, claim platforms, laboratories, pharmacies, medical devices, and external partners. This layer validates incoming data, enforces standards, and converts disparate formats into consistent structures. Interoperability frameworks such as FHIR and HL7 support this process. Well-designed ingestion pipelines remove duplication, apply governance rules, and create a transparent record of how data flows across systems.
Data storage has evolved beyond traditional warehouses and unmanaged data lakes. Warehouses handle structured data efficiently but struggle with scale and variety. Data lakes accommodate volume but often lack control. Modern architecture combines both approaches into governed Lakehouse environments. Clinical records, claims data, device feeds, and unstructured notes coexist under shared access policies. Encryption, partitioning, and role-based permissions protect sensitive information while supporting real-time analytics.
Data processing and modeling refine stored information into usable assets. Processing pipelines standardize values, align vocabularies, and prepare datasets for consistent use across the organization. Shared clinical terminologies such as SNOMED CT and LOINC ensure that metrics retain meaning regardless of source. This layer also resolves patient, provider, and payer identities into traceable relationships, creating the foundation for population analysis and quality improvement initiatives.
Analytics and activation translate curated data into operational impact. Dashboards, forecasting models, and automated workflows operate from the same trusted source, reducing disagreement and delay. Hospital leaders monitor resource utilization as conditions change. Payer teams identify claim anomalies early. Clinical programs prioritize outreach based on emerging risk patterns. Data becomes embedded in daily decisions rather than confined to retrospective reporting cycles.
Governance, security, and compliance anchor the entire framework. Clear policies define access rights, retention standards, and change management procedures. Encryption, authorization controls, and monitoring systems protect information across its lifecycle. Compliance requirements demand transparency and auditability. Strong governance reinforces consistency while reducing exposure as data ecosystems expand.
Building an AI-Ready Foundation
Artificial intelligence depends on disciplined data foundations. Algorithms reflect the quality, consistency, and lineage of the information that feeds them. AI-ready architecture therefore begins long before model development.
Organizations that invest in unified metadata management and continuous data validation experience faster returns from advanced analytics. Predictive risk scoring, utilization forecasting, and clinical decision support all rely on the same architectural rigor. Modern healthcare big data architecture must handle scale and diversity while preserving explainability. When data origins and transformations remain visible, analytical outputs earn trust and adoption.
Common Pitfalls in Modernization Efforts
Several patterns frequently slow data architecture initiatives. Some organizations integrate systems before defining governance, introducing inconsistencies that surface later. Others migrate workloads to the cloud without optimizing storage and processing, leading to rising costs and sluggish performance. Excessive customization creates long-term maintenance challenges and limits scalability.
Successful organizations approach data architecture as an evolving capability. Governance begins early. Data models remain standardized. Technical investments align with measurable clinical and financial outcomes. The objective centers on enabling insight, adaptability, and accountability rather than infrastructure expansion alone.
Looking Ahead
Designing healthcare data architecture for 2025 requires both precision and alignment. Organizations benefit from assessing current maturity, identifying redundancies, quality gaps, and compliance risks. Modernization efforts then focus on consolidating storage, strengthening interoperability, and automating integration. Activation follows through analytics, decision support, and AI-driven workflows that reach teams across the enterprise.
Hospitals, payers, and health technology providers that follow this progression shorten reporting cycles, improve coordination, and strengthen confidence in data-driven decisions.
Conclusion
Healthcare organizations stand at a data crossroads. Information flows from more systems than ever before, yet meaningful intelligence depends entirely on architectural discipline. A clear, unified framework brings order to complex data across the organization. It supports analytics, automation, and AI initiatives at scale for clinical, financial, and operational teams.
Leaders who prioritize modern data architecture build environments that support faster decisions, stronger compliance, and sustain improvement over time. The transformation begins with structure. For teams evaluating next steps, guidance from Healthcare Data Analytics Services offers practical insight into how modern frameworks support performance, governance, and reliable care delivery across evolving healthcare ecosystems.